22 May 2023
A microbiologist’s legacy: Safeguarding antibiotics to protect children
“Obtaining funding for research is always a challenge,” said Dr Stephanie Neville, a Research Fellow in bacteriology at the University of Melbourne’s Department of Microbiology and Immunology.
The late Dr Doris Mary Graham was also very aware of this challenge. A former senior lecturer in the Department, she chose to establish a legacy of support through a gift in her Will to enable important research projects such as Dr Neville’s.
Dr Graham was a keen traveller, ornithologist, and beloved sister to her three siblings. But she also had a lifelong career as a passionate microbiologist.
Starting her journey at the University of Melbourne, Dr Graham completed a Bachelor of Science in 1952. After completing a PhD and further research in London, she was recruited back to the University as a senior lecturer in the late 1960s.
One of Dr Graham’s career highlights was undertaking field work with Fred Hollows AC in remote Australian Indigenous communities, so it is fitting that this gift in her Will now funds research that will be of particular benefit to Australian Indigenous children.
Global and local impact
Dr Neville’s research team is investigating the bacteria that cause middle ear infections primarily in children. They’re examining how to address the growing problem of antibiotic resistance in these bacteria.
“The incredibly generous gift from Dr Graham has allowed my students and I to greatly expand our research program to include a breadth of clinical isolates from additional species of bacteria,” said Dr Neville.
“This has allowed us to better understand middle ear infection complications caused by antibiotic resistance.”
“Middle ear infections are incredibly common in all young children and in many cases can be cleared with a course of antibiotics. However, increased prevalence of antibiotic resistant strains is leading to treatment failure in a greater number of cases.”
Dr Neville said she is passionate about this area of research as the incidence of middle ear infections in children is astoundingly high.

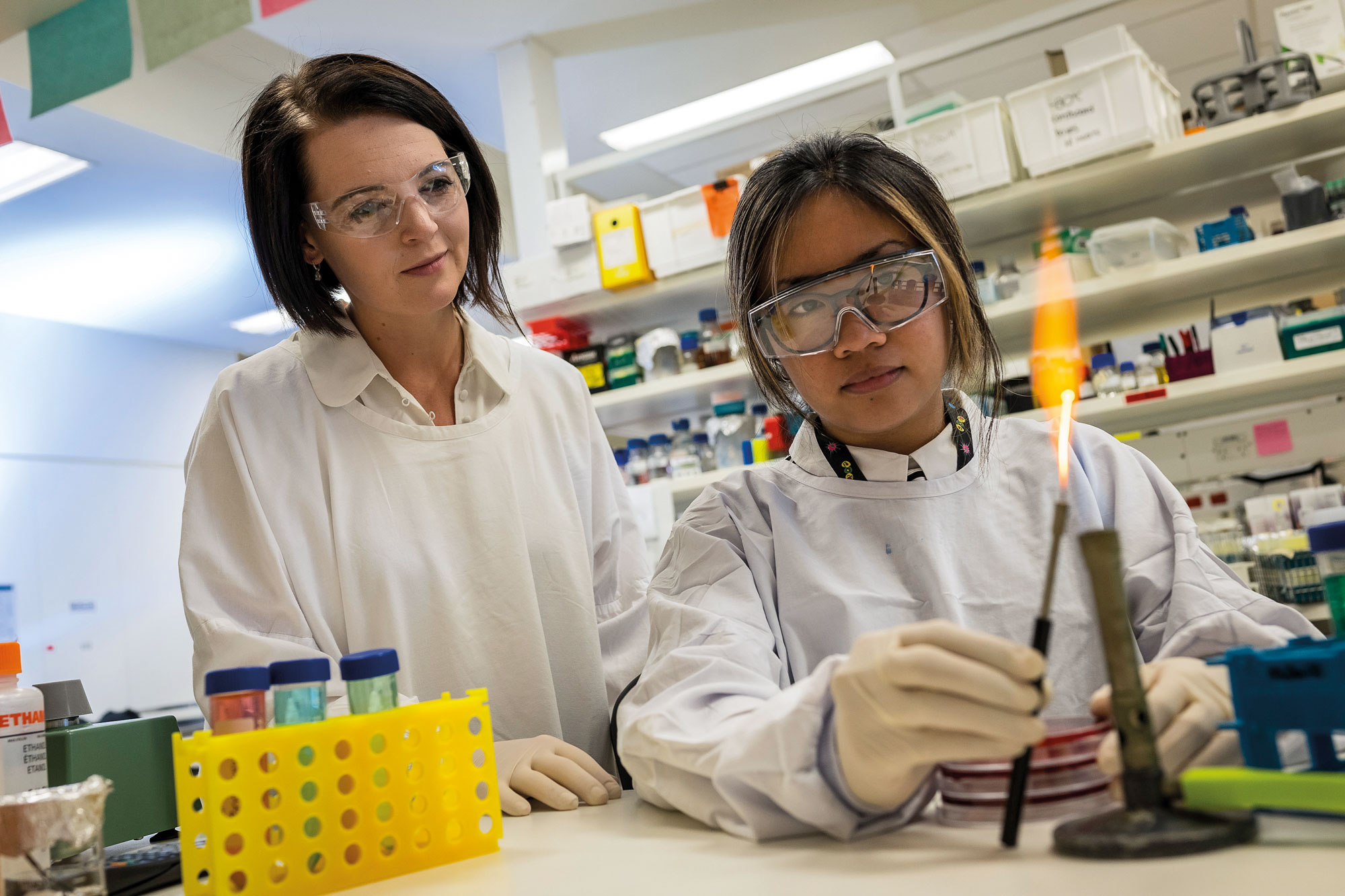
Dr Stephanie Neville in her lab at the Doherty Institute.
"There are roughly 700 million cases every year globally. Sadly, severe disease outcomes are generally over-represented in Indigenous Australian children who have one of the highest disease burdens of middle ear infections in the world."
An increasingly antibiotic resistant type of bacteria – Streptococcus pneumoniae – is responsible for a large proportion of these cases.
“The result of antibiotic treatment failure is that infections are lasting longer, increasing the chances of long-term damage, such as hearing loss, learning difficulties and speech impediments,” explained Dr Neville.
Rescuing crucial antibiotics
As a bacteriologist, Dr Neville wants to develop non-surgical treatment options for middle ear infections. But with the looming issue of antibiotic resistance, this is not a straightforward process.
“It generally takes a minimum of 5-10 years and millions of dollars to generate new antibiotics, most of which are rendered ineffective by antimicrobial resistance,” explained Dr Neville.
“Our research is attempting to rescue our current pool of antibiotics rather than developing new compounds. We aim to do this by breaking antimicrobial resistance in the bacteria that cause middle ear infections.”
Through her team’s work, Dr Neville has shown that the human body uses high concentrations of metal ions, such as zinc, to intoxicate invading bacteria.
“Interestingly, when we therapeutically enhance this metal ion intoxication, we see that many bacterial species become resensitised to antibiotics that they were previously resistant to,” said Dr Neville.
Using this knowledge, Dr Neville aims to develop a therapeutic strategy of combining current antibiotics with a metal-shuttling compound that will enhance the body’s natural metal ion intoxication process and improve the existing antibiotics’ efficacy.
Maintaining simple and effective treatments
A simple and non-invasive solution to the growing threat of middle ear infections is critical to the management of vast numbers of children who are affected each year.
As a result of the late Dr Graham’s gift, Dr Neville’s therapy could help many families avoid the devastating effects of treatment failure and give more children the opportunity to reach their full potential without disability or learning difficulties.
“Ultimately, we hope to use this research to develop a treatment regimen where these compounds can be coadministered with antibiotics to patients as standard practice,” said Dr Neville.
“This will allow patients who are carrying antibiotic resistant strains to be cured quickly and effectively without the risk of treatment failure.”
Best of all, the treatment would be simple and easy to access, helping more children avoid hospitalisation in the first place.
“Based on our current findings, we anticipate that this treatment will be available in much the same way as current antibiotics. It will require a script from a GP and a course of oral medication,” said Dr Neville.
Building on fundamental research
Ultimately, Dr Neville knows her research is not only helping children with middle ear infections, but also contributing to a much broader and largely unknown complication.
“It’s very easy to take our access to medication for granted. More than that, we have come to expect that when we do need medication, it will work – but the issue of antibiotic resistance is much greater than most people realise,” said Dr Neville.
“We need to make sure that antimicrobial medication will continue to be available and effective; that’s ultimately what this research to aims to achieve.”
Dr Neville is grateful for the opportunity to build on the work of other microbiologists – including that of Professor Christopher McDevitt who she continues to work alongside at the Peter Doherty Institute for Infection and Immunity (the Doherty Institute).
“All of this work has arisen from many years of fundamental bacteriology research, which is vital for continued therapeutic translation,” said Dr Neville.
Dr Graham’s gift in her Will has allowed Dr Neville and her team to efficiently pursue this critical medical research and build collective knowledge around fighting antibiotic resistance.
“I am incredibly grateful to Dr Graham for her passion and dedication to biomedical research and the discipline of microbiology,” said Dr Neville.
"It’s a very noble decision to bequeath a gift to medicine. I hope she would be proud of the research that her generosity has enabled."
This article was first published by University of Melbourne
Funding: Dr Graham’s bequest builds on the funding Dr Neville received from the Garnett Passe and Rodney Williams Memorial Foundation for her existing project: Breaking antibiotic resistance in otopathogens. This project addressed the critical issue of antibiotic resistance in bacteria that cause middle ear infections (otitis media), which are prevalent in Indigenous communities in Australia.


