10 Aug 2018
A strong immune system helps ward off colds and flus, but it’s not the only factor
First published in The Conversation
By Research Fellow Hui-Fern Koay, and PhD student Jesseka Chadderton from the Department of Microbiology and Immunology, The Peter Doherty Institute for Infection and Immunity.
It’s peak flu season. You’re cold, rugged up and squashed on public transport or in the lift at work. You hear a hacking cough, or feel the droplets of a sneeze land on your neck. Will this turn into your third cold this year?
No matter how much we try to minimise our exposure to respiratory viruses, it’s far more difficult in winter when we spend so much time in close proximity to other people.
On top of this, viruses tend to be more stable in colder and drier conditions, which means they stick around longer.
The common cold is caused by more than 200 different viruses, the most common of which are rhinoviruses (rhino meaning nose). Rhinovirus infections tend to be mild; you might get a sore throat and a head cold lasting just a few days.
Influenza, or the flu, is generally caused by type A or B influenza viruses. The flu is far more aggressive and often includes a fever, fatigue and body aches, in addition to all the classic cold symptoms.
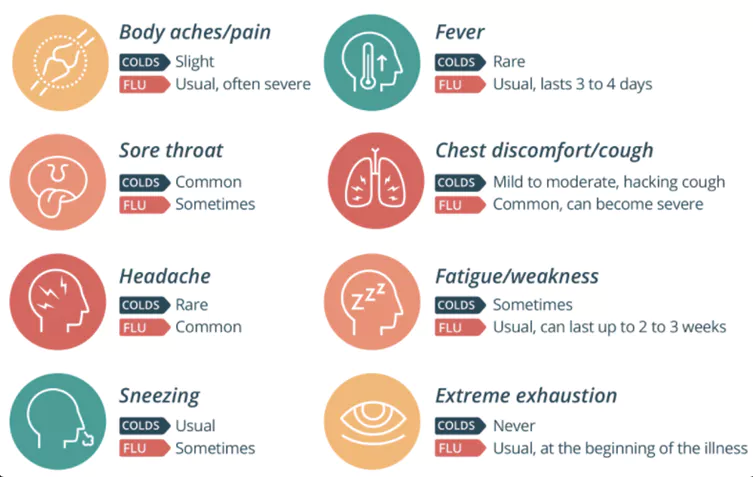
The flu tends to be more severe than the common cold. Image courtesy of healthdirect.
When it comes to getting sick, there’s always an element of bad luck involved. And some people, particularly those with young children or public transport commuters, are likely to come into contact with more viruses.
But you may have noticed that illness often strikes when you’re stressed at work, not sleeping properly, or you’ve been out partying a little too much. The health of our immune system plays an important role in determining how we can defend against invading cold and flu viruses.
How the immune system fights viruses
Your skin and saliva are key barriers to infection and form part of your immune system, along with cells in every tissue of your body, including your blood and your brain.
Some of these cells migrate around to fight infection at specific sites, such as a wound graze. Other cells reside in one tissue and regulate your body’s natural state of health by monitoring and helping with the healing process.
The cells that make up your immune system need energy too, and when you’re low on juice, they’ll be on low-battery mode. This is when our natural immune defences are weakened and normally innocuous bugs can begin to cause strife.
Our immune system requires a lot of energy to defend our bodies. Feeling tired and achy, overheating, and glands swelling are all signs that our immune system is busy fighting something.
Boosting our natural defence system
Our immune system has evolved to naturally detect and eliminate viral infections. And we can actively strengthen our immunity and natural defences by looking after ourselves. This means:
- getting adequate sleep. Sleep deprivation increases the hormone cortisol, which suppresses immune function when its levels are elevated
- exercising, which helps the lymphatic system, where our immune cells circulate, and lowers levels of stress hormones
- eating well and drinking enough water. Your immune system needs energy and nutrients obtainable from food. And staying well hydrated helps the body to flush out toxins
-
not smoking. Smoking, or even secondary smoke, damages our lungs and increases the vulnerability of our respiratory system to infection.
Educating our immune system
Natural defences aren’t always enough to keep us safe and we need the help of flu vaccinations.
Vaccines are designed to educate an army of B and T cells which make up your adaptive immune system. This arm of your immune system learns by exposure and provides long-term immunity.
These T and B cells need a bit of time from the initial influenza exposure before they can be activated. This activation lag time is when you feel the brunt of the flu infection: lethargy, body aches, extreme fatigue and unable to get off the couch for a day or two.
To overcome this delay and protect people before they are exposed to potentially harmful flu strains, flu vaccination introduces fragments of the influenza virus into the body, which acts like prior exposure to the bug (without actual infection).
Seasonal vaccines are designed to match currently circulating strains and target those strains before you’re infected.
You can still catch the influenza virus if you are vaccinated. But because of this pre-education, the symptoms will likely be milder. The immune system has been trained and the army of B and T cells can move into action quicker.
Already have a cold or the flu?
If you’ve been sniffling and sneezing your way through winter, be comforted by the fact that these bugs are strengthening your immune system. Our body remembers the particular strain of rhinovirus or influenza we get, so it can recognise and mount a stronger defence if we encounter it again.


