04 Aug 2021
COVID-19 - The Israel experience
By Dr Neta Petersiel, Clinical Research Fellow for ASCOT
This blog first appeard on the AustralaSian COVID-19 Trial (ASCOT) website
The past 18 months often feel like a weird dream, our reality perhaps forever changed by a virus. We are now used to speaking about COVID “waves” and lockdowns, wearing surgical masks and practicing social distancing. While the pandemic has affected the entire world, it has taken a different course in each country. Here, I share with you the unique aspects of the pandemic in Israel and some of my personal experiences dealing with it.
The first COVID-19 cases in Israel were diagnosed in March 2020. I first started working as an attending physician on the COVID-19 ward at the Rambam Health Care Campus (RHCC) in July 2020 as the second wave started picking up. At my hospital, we’ve tried to continue our routine medical work alongside COVID-19 as best we could. At the beginning of July, we had six general medical wards and a single COVID-19 ward. By September, we were in what felt like a tsunami of cases, and we had to open more and more COVID-19 wards.
By the end of the month, we had five medical wards and four COVID-19 wards (that’s three extra wards in case you’ve lost count). At that point we had exhausted all the spare rooms in the hospital, and we were short on staff. A decision was made to move all COVID-19 wards into the fortified hospital in the underground parking lot. You’ve read it right – the parking lot. As if COVID reality wasn’t surreal enough, we had started admitting patients into spaces that were recently occupied by cars. Just try to imagine what you would feel like as a patient, admitted to a car spot, being cared for by staff in outer-space looking suites.
Surprisingly, this solution worked well, and with the added space, families were allowed to visit daily in the COVID-19 compound, which was great for the patients’ well-being. The staff shortage was solved with the aid of the Israeli Defense Force (IDF) who came to our rescue and opened a COVID-19 ward using army doctors and nurses. It was quite a big change for them to be caring for elderly patients with COVID and other medical conditions, instead of healthy soldiers. It was a joint effort, and I guess now is a good opportunity to thank them for their hard work.
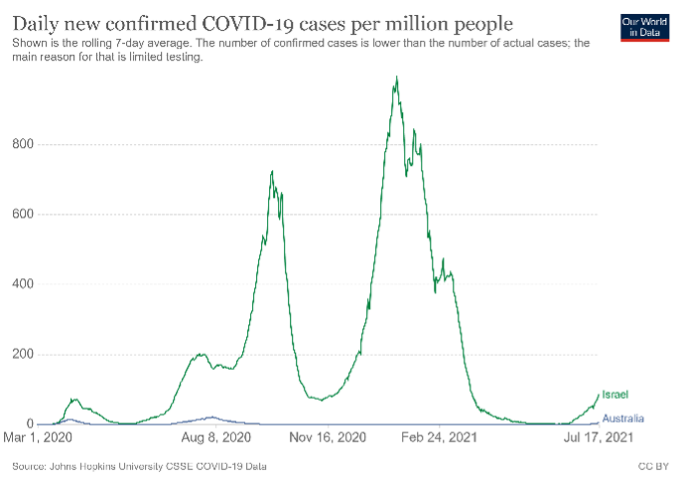
COVID19 “waves”, Israel (green) and Australia (blue)

Rambam Health Care Campus underground COVID19 hospital
The other unique aspect of the pandemic in Israel was the massive vaccination campaign led by the Ministry of Health. Early during the pandemic, as many pharmaceutical companies were developing vaccines, the Israeli government decided to bet on them all, buying large stocks of each vaccine. As we now know, it was Pfizer that crossed the finish line first, followed closely by Moderna. Days after Pfizer announced their results, our local vaccine campaign started.
The scheme was simple, get vaccinated and receive benefits. For example, you could travel abroad, visit hotels and venues, and if you happened to be exposed to a COVID-19 case, you didn’t need to self-isolate. This is on top, of course, of reduced chances of catching a dangerous virus and protecting your family and community. In fact, so many people wanted the jab that long lines formed, and we were afraid that we wouldn’t keep up with the high demand.
At the peak of the campaign, over 150,000 vaccine doses were given each day around Israel. This necessitated a well-oiled machine that could supply the vaccines, and this is where the four Israeli health maintenance organisations came into the picture. These organisations serve as both the insurer and the medical providers for all Israeli citizens. They have a long tradition of preventative medicine (i.e. vaccinations) and are broadly dispersed geographically. To further improve their services, drive-in centres for vaccinations opened, where you simply had to drive in your car, open the window and get the jab.
Three months into vaccination, about 60 per cent of the population was vaccinated, on top of 850,000 people who had COVID-19, leading to a total of 72 per cent of our population with some immunity (either naturally or by vaccination). Among the most susceptible population, the elderly, the vaccine coverage has been even more impressive as can be seen in the table below.
With the spread of the Delta variant, we are currently witnessing a fourth COVID-19 “wave”. At least for now, even with the numbers rising, we are not yet seeing a significant increase in the number of hospitalised patients. It seems that we haven’t heard the last from this nasty virus yet.
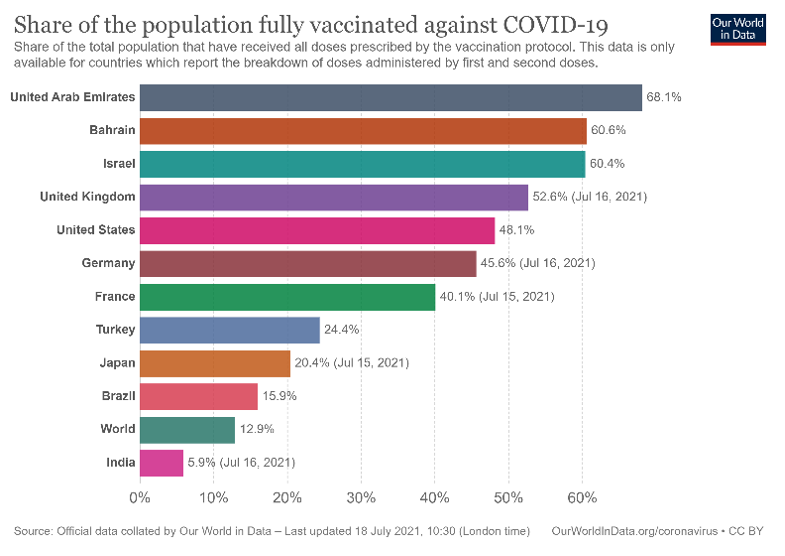
Share of population fully vaccinated against COVID-19
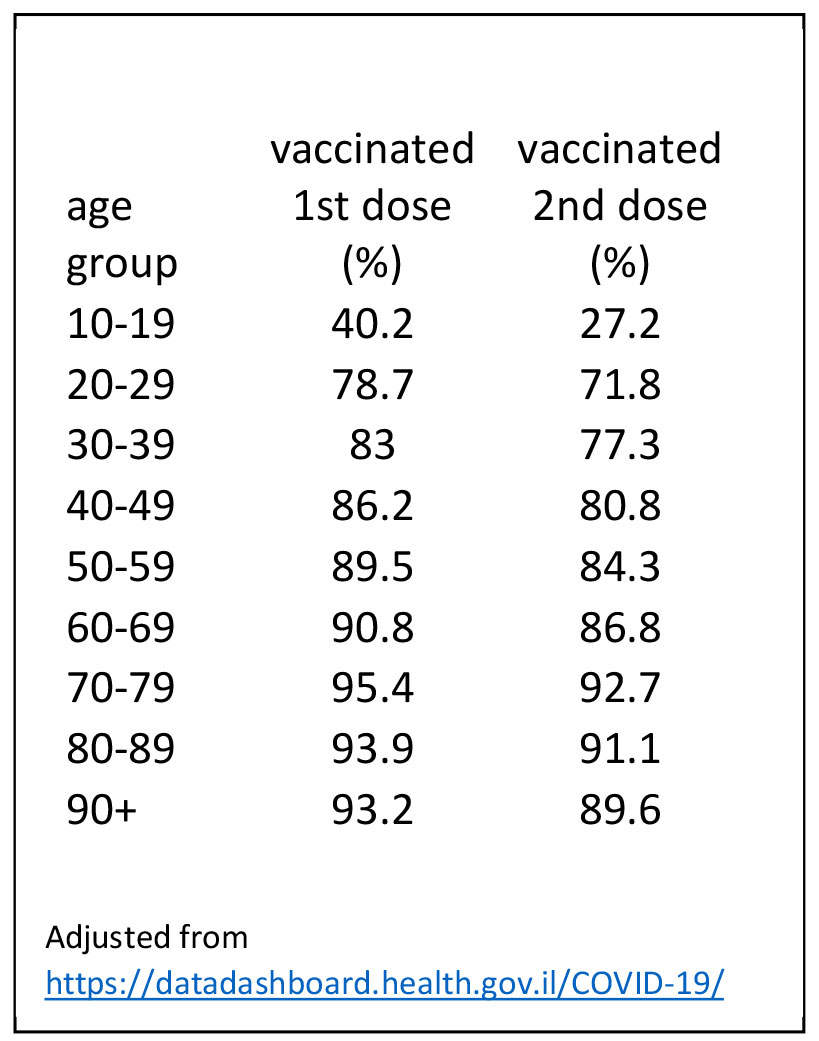
Vaccine uptake in Israel by age group


