06 Jul 2020
Meet the scientist – Q&A with Associate Professor Siddhartha Mahanty
Q: What is your role at the Doherty Institute?
I'm an infectious disease specialist, doing both clinical and lab research.
Q: What initially attracted you to the field of science and, specifically, infectious diseases?
I received my medical training years ago in Sydney at New South Wales University, and went on to Australian National University in Canberra for basic clinical and internal medicine training. There were very few infectious disease research opportunities available in Australia at the time, so I subsequently moved to the US where I ended up finishing my infectious disease training in Cleveland, at Case Western Reserve University. After my clinical training, I was able to stay on in the US firstly to complete a postdoctoral fellowship in a leading parasitology laboratory at the National Institutes of Health (NIH) in Bethesda, MD, where I became very interested in studying worms and then moved on to a career as infectious disease specialist.
Q: Why did you choose to focus your research on worms?
When some people hear about worms they go ‘eww!’ but others find it fascinating. I’m part of the latter group of people, sometimes called nerds!
During my postdoctoral fellowship, there was a project that was related to a worm that causes filariasis, which is commonly recognised as the condition called elephantiasis. This tiny worm is transmitted by mosquitoes and lives in the lymphatic system of humans, causing severe progressive swelling, particularly in the legs. I found the biology and immunology of worms so fascinating. They’re multicellular organisms that can live within another organism for years without being killed or rejected by the host. I investigated this phenomenon as a postdoctoral fellow and continued to investigate it for years.
During the nineties however, my focus changed for a while to viral immunology, studying viruses rather than worms, because funding was much better in virology at the time. I worked primarily on the immunology of Ebola and Lassa viruses. It was a very relatively new area of investigation at the time in the early 2000s. I worked in BSL4 (high containment level) labs at the Centers for Disease Control and Prevention in Atlanta and went out to two Ebola outbreaks in Africa as a member of CDC teams. It was an interesting period in my career, but my primary love has always been research into worms and parasites. So when I got a chance to get back into worms, I did, and returned to the NIH in a staff position, where I was before moving to Melbourne in 2017.
Q: What are you currently working on?
Currently, there are two areas of work I’m focused on. In the lab, I’m working on projects aiming to understand the mechanisms by which severe malaria causes damage to the human host. It's a different type of a parasitic infection when compared to worms. The project that I'm working on is trying to determine a role for small molecules called microRNA, that regulates gene expression within the parasite and within the host.
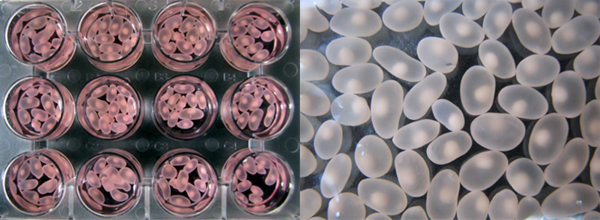
T. solium cysts recovered from naturally infected pigs in Peru.
Q: What's the biggest challenge in this research?
Firstly, I want to understand how the worms manipulate the immune system. This is a crucial step in the survival of the pathogens. What tools do they use? Most of the time, these immune systems are regulated by small molecules and proteins that stimulate or inhibit immune cells. The worms are inducing production of these proteins that are effectively braking or slowing down the inflammatory immune cell population. Secondly, I don't have a full catalogue of what these proteins are. Having such a catalogue would be very helpful in designing treatments or therapies to stop that break down and allow the host to respond in a normal, damaging immune response, which would then kill the worm. So we need to understand the small molecules in order to do this manipulation.
Q: Has COVID-19 impacted your work?
Since January and throughout the COVID-19 pandemic, I have been involved in studies of infections in healthcare workers at the Royal Melbourne Hospital. Being an infectious disease specialist with clinical training, I have a lot of interest in infectious disease in general and, with my previous experience working with Ebola and Lassa, this outbreak felt like a good opportunity to contribute. The purpose of the study is to understand what happens in the early few days after infection with COVID-19, by following a group of healthcare workers who are highly exposed to the virus via their patients and dissecting their immune response if they are infected.
Q: What would you say is your greatest hope for your research and what have you done to date that you're most proud of?
I'm most proud of the work that I've done with tapeworm immunobioilogy and understanding the way the immune system is regulated by the tapeworm, both for the survival of the worm and explaining the damage that it does to the host. It was a body of work that spanned from 2011 to 2017 when I was at the National Institute of Health in the US and a lot of the work was done in collaboration with very enthusiastic and bright young scientists in Peru. I feel good about having trained people in that environment, giving them opportunities to develop their scientific skills.
I think all of us hope that we can get control of infection and disease worldwide. That control is going to take a combination of efforts in anti-parasitic treatment and public health measures to improve the condition of people, as well as vaccine development. If research in any of those fields can make big strides forward, I think it will be a major achievement over the next five to ten years.


